What The Fifty Podcast – Episode 59: Affairs of the heart
We’re talking affairs of the heart with the enigmatic Dr. Claudine Lewis (@heartsmartja). Plus, we’re throwing in some travel stories you’re going to love! Tune in now!
We’re talking affairs of the heart with the enigmatic Dr. Claudine Lewis (@heartsmartja). Plus, we’re throwing in some travel stories you’re going to love! Tune in now!
At age 36, Dionne Nesbeth was diagnosed with diabetes, and months later she experienced two heart attacks that resembled a case of indigestion.
“I started feeling chest pains and thought it was indigestion. I didn’t take it as anything because at 36, I told myself I am too young to have a heart attack,” the Heart Smart Centre Wear Red ambassador, who speaks on behalf of the many women beset with heart disease in Jamaica, told a gathering during a reception earlier this month.
In fact, instead of visiting the doctor after fainting, Nesbeth said she decided to rest because she felt her condition was caused by something she must have eaten. She even drove herself home after the fainting subsided, because, again, “At 36, I couldn’t be experiencing a heart attack” she convinced herself.
It was not until she started having some serious chest pains and numbness in her left arm that she decided to check it out.
Nesbeth’s case is not unique says cardiologist Dr Claudine Lewis, but the disbelief she experienced may have been bolstered by the images portraying heart disease. “The images advertising heart disease is usually a man holding his chest,” she states.
Her aim is to raise awareness among women that this is something that affects them equally. “And not just heart attacks, we are talking about every single kind of heart disease, which is not discriminatory as it relates to gender or age,” she argued.
“You have heart disease from you are born, all the way up to a child … . We talk about living healthy lifestyles, and must remember that there are heart conditions that we have no control [over]. A rhythm abnormality, for instance, is not something you can eat yourself out of,” said Dr Lewis.
However, these are things that can be picked up early with a screening test, said the cardiologist, who argues that there is not enough information about heart disease in women, unlike the efforts placed in building awareness around breast cancer, for example.
Dr Lewis says she is prone to heart disease because of her strong family history and high cholesterol, although she is slim, so she does routine screening.
She was able to get three of her patients, Nesbeth, Venetta Smith-Bowen and P.J. Stewart, to become Heart Smart Centre Wear Red ambassadors during the week leading up to February 3.
HEART ATTACK MISTAKEN FOR GAS PAINS
Smith-Bowen, at age 33, thought she was having gas pains so she drank tea. However, she became concerned quicker than Nesbeth and decided to visit the doctor, who did an electrocardiogram (ECG) and found abnormalities. “He referred me to do an echocardiogram, which I did. during that test it showed I had a leaking valve in 2011.”
She said she went about her business normally, because for her the idea of doing surgery was a “no-no”.
In 2020, she started feeling pain in her stomach, back, other parts of her body, except for her chest. “Weakness in the legs, sometimes swelling, and back and forth to the doctor,” said Smith-Bowen.
She decided to go overseas to spend time with her sister, and while home alone she passed out. When her sister found her, she was conscious but weak. By the time she got to the hospital her situation had worsened, and while doctors were doing a test she passed out again and went into a coma.
Her sister signed for the surgery she never wanted to do all these years. She was unconscious for six days.
Today, at 45, her lifestyle has changed. Her eating habits have changed, and she now walks three miles in the mornings. Before, she would walk and tire. “Two heart valves were leaking, they replaced one and they repaired the other. If you come close to me sometimes you can hear one going tick, tick, tick, tick,” she quipped.
Smith-Bowen can laugh today about her condition because she is far more aware, and she is on heart-saving medication.
Nesbeth says she was referred to Dr Lewis, who told her that life did not stop because she had two heart attacks. “I was fretting. I was fearful, because I have heard so many stories of people not living through heart attacks. But Dr Lewis told me that the treatment you receive right after a heart attack is very important.”
She has done an angioplasty, which is where doctors open the arteries with a stent to allow blood flow.
A heart attack is a blockage of one or two arteries inside the heart restricting blood flow.
She admits it has not been easy changing her diet, but gradually the body becomes in tune with the person eating better.
Both women take several pills to stay alive as well, and they are happy.
Heart Smart Centre Goes Red” was the theme for Montego Bay-based cardiologist Dr Claudine Lewis’s latest initiative to highlight and promote heart health in women. The initiative included two events on Friday, February 3, a heart health screening exclusively for women and a Wear Red cocktail event.
“We decided to stage Heart Smart Centre Goes Red to raise awareness about heart disease in women. As a woman cardiologist, and someone with heart disease risk factors, it is particularly important to me and our team to highlight how heart disease behaves differently in women. Our awareness campaign introduces our Red Dress ambassadors, who have been engaging women to get screened by sharing their heart health stories. We have also dedicated our team to screening female members of our community for heart disease and heart disease risk factors,” Lewis explained.
The Wear Red cocktail event saw the entrance to Heart Smart Centre, located on G West Centre in Montego Bay, transformed by event décor outfit Tai Flora Services. The relaxed ambiance saw guests from the medical, political and business sectors; leisurely imbibing sips of vino from Select Brands and CPJ, paired with tasty bites from Stush in the Bush and Rainforest Caribbean. Guests were also treated to entertainment from singer Alexandria Love and the Good Vibes Ongle Band.
The Heart Smart Centre in Montego Bay, St James, team led by cardiologist Dr Claudine Lewis, will offer free cardiovascular disease risk assessment exclusively to women in western Jamaica in observance of Wear Red Day ®, Friday February 3. Wear Red Day®, an American Heart Association initiative is a global campaign, dedicated to raising awareness about heart disease in women. As cardiovascular disease numbers rise worldwide, Dr Lewis notes that the health fair is critical now more than ever, as it would serve to raise awareness about cardiovascular disease, while providing women with an opportunity for early detection.
Current estimates from the World Health Organization (WHO) are that over 17 million people die from the disease worldwide annually. This includes heart attacks, strokes, and peripheral vascular disease. Fifteen years ago, this represented 30 per cent of all global deaths. That number is growing and is expected to double by 2030, Dr Lewis pointed out.
She noted that in Jamaica, cardiovascular disease remains one of the leading causes of illness and death. “Women account for more than 50 per cent of this number. Within the medical community we know there are sex-based differences in how men and women express signs and symptoms of heart disease.” She continues, “Women may not have typical symptoms of heart attack, for example, and can sometimes be dismissed as being anxious and diagnosis can be delayed.” Hence, this mission to raise awareness about these differences and to help women recognise the signs and symptoms of heart disease as well as to get screened for silent heart disease or risk factors for heart disease such as hypertension, high cholesterol, and diabetes.
RED DRESS AMBASSADORS
As part of the awareness campaign, the centre will be introducing HSC red dress ambassadors.
Red dress ambassadors are women who have been diagnosed with and treated for heart disease and have been living full lives. The women will share their stories of how they found out they had heart disease, treatments they have undergone and what it’s like to live with the diagnosis of a heart condition.
To benefit from the free screen, participants must wear red to the screening. Only women participants will be screened. Participants will complete a heart health questionnaire, and have free blood pressure, body mass index, blood sugar and cholesterol checks. The first 15 participants with abnormal screens will also receive free electrocardiograms and all participants with an abnormal heart screen will be reviewed by our cardiologist with follow-up recommendations, a release from the centre notes.
WESTERN BUREAU:
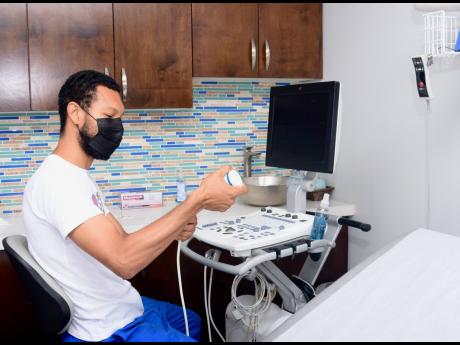
The Heart Smart Centre in Montego Bay, St James on Thursday, September 29 provided heart disease screening for residents, including free electrocardiogram tests for the first 20 registered patients, as part of its observance of the globally celebrated World Heart Day.
From as early as 9 a.m., youthful and elderly patients alike waited to be seen at the Heart Smart Centre’s office at the GWest Medical and Surgery Centre in Montego Bay’s Fairview business complex, eager to find out whether they would get clean bills of heart-health or get recommendations for further tests and screening.
In addition to having their hearts examined, patients also got to check their body weight and body mass index, blood pressure, and blood sugar as part of their overall wellness checks.
Zoie Porter, one of the first 20 patients, who were provided the screening free of cost, praised the Heart Smart Centre for hosting the health fair.
“I think it is a good initiative, because it helps you to know the status of your heart. You might be getting up every day and going about your daily business, and you’re getting no signal that anything is happening to you,” said 67-year-old Porter. “If you come to these health fairs, you can know what is going on with you, and you can take it from there by following up with your doctor and then you can live a healthy lifestyle, and I made sure to get the free check-up because I am a health freak.”
Angela Eccleston, another patient who came for her heart check-up at the health fair, said that her screening process was positive due to the relative swiftness of the procedure and the staff members’ kind and professional attitude during each segment of testing.
“I was just passing by and I saw the persons here, and I was wondering what it was about. When I heard about what was going on, I said that there is nothing wrong in getting checked,” said Eccleston. “The wait was not long at all, as I got through quickly, and thank God my heart is normal. Everybody was kind and courteous, and you could chit-chat with them while going through the checks.”
The Heart Smart Centre’s health fair was held at a time when the World Health Organisation (WHO) has estimated that over 17 million people worldwide die from cardiovascular disease each year, to include heart attacks, strokes and peripheral vascular disease.
Dr Claudine Lewis, a licensed cardiologist and the overseer of the Heart Smart Centre, told The Gleaner that approximately 20 per cent of Jamaicans have heart-related issues, many of which are linked to high blood pressure and diabetes.
“From the statistics that we have, it would be 20 per cent of the population that has heart issues, and most heart-related disease is driven by high blood pressure. That is why we try to focus on high blood pressure as a screening measure, because out of the population, about 20 to 25 per cent of all Jamaicans have high blood pressure,” said Lewis.
“There is a common misconception that persons will feel sick or get a headache to know that their pressure is high, but most of the time people have high blood pressure and they do not know. Diabetes and high blood pressure are the main risk factors for heart disease, and diabetes is considered to be a coronary heart disease equivalent,” Lewis added.

ST JAMES, Jamaica – Scores of individuals streamed into the Heart Smart Centre Limited at the GWest Medical Centre in Montego Bay, St James, for free heart disease screening to mark World Heart Day, celebrated on September 29 each year.
After registration, the individuals got their weight, height, blood pressure and blood sugar checked at the health facility.
They were subsequently sent home, if results of the checks prove to be normal, but were directed to Dr Claudine Lewis, cardiologist at Heart Smart Centre, for further evaluation if any abnormalities are detected.
“The whole part of screening is to pick up people who may have symptoms, or may be at risk, whether through family history, or maybe they have something like high blood pressure, that have no symptoms; pick them up and then we put them on the path for having further evaluations,” explained Dr Lewis.
She was elated over the overwhelming turn-out for the free evaluation offered by Heart Smart Centre.
“The response from our guests have been amazing, they really appreciate the experience. It’s a little bit hectic because it’s a lot of people who have tried to access the services today but we have worked out some of the kinks and so far it’s pretty good. We are at 75 now in terms of persons who have registered….with all the rain and everything,” the cardiologist said.
After accessing the service, a 70-year-old Montego Bay woman, Monica Bennett, was found with abnormalities. She used the free service to verify a similar diagnosis at the health clinic.
“It’s okay. I am glad about getting the opportunity to do it because sometimes you don’t have the money to do it. And I am glad about it. They told me that I have a problem with my heart so I need to see a specialist. My doctor at the clinic already told me, but I am happy for the second opinion,” Bennett said.

We hear the very tragic story of a young star athlete who was playing sports and collapsed suddenly on the field and died, or died in sleep without any knowledge for any medical problems. Most often, these cases are caused by sudden cardiac arrest. People often use these terms interchangeably, but they are not synonyms. A heart attack is when blood flow to the heart is blocked, and sudden cardiac arrest is when the heart malfunctions and suddenly stops beating unexpectedly. A heart attack is a “circulation” problem and sudden cardiac arrest is an “electrical” problem.
What is a heart attack?
A heart attack occurs when a blocked artery prevents oxygen-rich blood from reaching a section of the heart. If the blocked artery is not reopened quickly, the part of the heart normally nourished by that artery begins to die. The longer a person goes without treatment, the greater the damage. Symptoms of a heart attack may be immediate and intense. More often though, symptoms start slowly and persist for hours, days or weeks before a heart attack. Unlike with sudden cardiac arrest, the heart usually does not stop beating during a heart attack. The heart attack symptoms in women can be different than men.
What is cardiac arrest?
Sudden cardiac arrest occurs suddenly and often without warning. It is triggered by an electrical malfunction in the heart that causes an irregular heartbeat (arrhythmia). With its pumping action disrupted, the heart cannot pump blood to the brain, lungs and other organs. Seconds later, a person loses consciousness and has no pulse. Death occurs within minutes if the victim does not receive treatment.
True story
So about one year ago, I was “on-call” for the hospital, it was early in the morning, around 7am, when a friend of mine called from the airplane – the were boarded and just about to take off when a passenger slumped over beside his wife. She immediately called for help and it was noted that the passenger was not responsive. Fortunately a doctor was on the flight and jumped into action quickly starting to provide hands-only CPR. My friend called me, not knowing I was on call, but she was shaken up by what had happened and just wanted to talk. After listening, I told her I’m going to go, because I’m pretty sure in they will be calling from the emergency room (ER) soon about this man… no sooner than I said that – my emergency phone beeped.
When I got to the ER, it turns out the passenger had a massive heart attack which then led to a cardiac arrest. So sometimes the two can be linked, but they are not one in the same. Most of the times when you hear of athletes, or some other young person without any known medical history collapsing and dying suddenly – it is usually because of a cardiac arrest – because the heart has gone into an abnormal rhythm, and not a heart attack.
What is the link?
These two distinct heart conditions are linked. Sudden cardiac arrest can occur after a heart attack, or during recovery. Heart attacks increase the risk for sudden cardiac arrest. Most heart attacks do not lead to sudden cardiac arrest. But when sudden cardiac arrest occurs, heart attack is a common cause. Other heart conditions may also disrupt the heart’s rhythm and lead to sudden cardiac arrest. These include a thickened heart muscle (cardiomyopathy), heart failure, arrhythmias, particularly ventricular fibrillation, and long Q-T syndrome.
Fast action can save lives. Find out what to do if someone experiences a heart attack or cardiac arrest.
What to do: Heart Attack
Even if you’re not sure it’s a heart attack, call for HELP or 119. . Every minute matters! It’s best to call an ambulance with trained emergency technicians to get to the emergency room right away. Emergency medical services staff can begin treatment when they arrive — up to an hour sooner than if someone gets to the hospital by car. Ambulance staff are also trained to revive someone whose heart has stopped. Patients with chest pain who arrive by ambulance usually receive faster treatment at the hospital, too.
What to do: Sudden Cardiac Arrest
Cardiac arrest is reversible in most victims if it’s treated within a few minutes. First, call for HELP or 119 for emergency medical services. Then get an automated external defibrillator if one is available and use it as soon as it arrives. Begin CPR immediately and continue until professional emergency medical services arrive. If two people are available to help, one should begin CPR immediately while the other calls 119 and finds an AED.
Sudden cardiac arrest is a leading cause of death – over 320,000 out-of-hospital cardiac arrests occur annually in the United States. By performing Hands-Only CPR to the beat of the classic disco song “Staying Alive,” you can double or even triple a victim’s chance of survival.
Learn Basic CPR
The Heart Foundation of Jamaica and other heart clinics offer Basic CPR, sign up today! and get certified. This is especially recommended if you have a relative or friend with a known heart problem.
 Heart Smart Talk
Heart Smart Talk
February 5th 2016
Heart Disease in Women
Each year in the United Stats and other countries, the month of February is observed as Heart Month. In Jamaica we observe heart month with several activities over the course of the month led by the Heart Foundation of Jamaica, the Cardiology Unit at the University Hospital of the West Indies and other cardiologists and heart centres promoting awareness of heart disease prevention and early detection and treatment. This year, the theme for heart month is Sudden Cardiac Arrest.
The first Friday of February is also typically observed as Go Red for Women day, raising awareness for heart disease in women in particular. This is because heart disease is typically believed to be a disease predominantly affecting men, but women are equally affected by heart disease and the symptoms tend to be less dramatic and typical and as a result are often ascribed to other diseases. This is of course close to my heart, as a woman and as a cardiologist taking care of women with heart disease.
My personal story is that I have been diagnosed with high cholesterol and have a strong family history of Hypertension. Though high cholesterol is not in itself heart disease and the link between some types of high cholesterol and blocked arteries is controversial at best, there is a lot of science supporting the role of high cholesterol in the development of atherosclerosis ( blocked arteries). Coupled with Hypertension and poor diet, a sedentary lifestyle and other risk factors such as diabetes and cigarette smoking, women can develop atherosclerosis at a young age. When I share my story with patients, they always say, “but doc, you are not fat”. That is the thing about heart disease in women, though obesity is a cardiac disease risk factor, many women who are of ideal weight are not the healthiest – hence the need for early screening for heart disease and heart disease risk factors in ALL women. In my particular case all the women in my family have high cholesterol and it seems we have familial high cholesterol – which is a genetic defect, affecting how the liver handles cholesterol. Learning about this has encouraged me to be more attentive to my diet and physical activity levels.
In the United States, 1 in 4 women dies from heart disease. The most common cause of heart disease in both men and women narrowing or blockage of the coronary arteries, the blood vessels that supply blood to the heart itself. This is called coronary artery disease and it happens slowly over time. It’s the major reason people have heart attacks.
Heart diseases that affect women more than men include
• Coronary microvascular disease (MVD) – a problem that affects the heart’s tiny arteries
• Broken heart syndrome – extreme emotional stress leading to severe but often short-term heart muscle failure
The older a woman gets, the more likely she is to get heart disease. But women of all ages should be concerned about heart disease. All women can take steps to prevent it by practicing healthy lifestyle habits.
Not all heart disease is preventable, there is some heart disease that women are born with – called congenital heart disease such as mitral valve prolapse, and “hole in the heart” conditions such as Atrial Septal Defects and Ventricular septal defects and more complex congenital heart disease. These congenital heart diseases though account for the minority of cases of heart disease, usually less than 5%. So acquired heart disease linked to unhealthy lifestyle choices and other risk factors account for the majority, which means you can do something to lower your risk of developing heart disease, or get tested early and regularly.
So what can you do?
• Know your numbers – get screened for heart disease by age 20 years old. This can be done with your family doctor, sit with your doctor and have them go through your history in detail and examine you thoroughly, adding some blood work – Blood glucose, cholesterol CRP(Marker of inflammation) to your evaluation. Additional testing such as ECG would be at the discretion of your doctor. If your initial screen is good, then your doctor would recommend follow-up every 5 years. At age 40, schedule at least an annual review.
• Keep moving! Plan to have do at least 150 minutes of moderate physical activity per week
• Eat well – eat a diet rich in fruits, vegetables, whole grain and low in processed foods and simple carbs
• Self-care – a buzz phrase for the last few years, but such an important aspect of life, particularly as a woman. We often put the interest of others – ahead of ours, and neglect self care. Take care of your emotional needs, have positive self-talk, rest well and check in with yourself often. Emotional stress is one of the leading causes of presentation to the cardiologist with symptoms of anxiety and depression.
Signs you may have blocked arteries or a heart attack.
A heart attack – known in medical jargon as a myocardial infarction or MI for short, occurs when plaque that has been building up in your coronary arteries rupture and a clot forms leading to sudden blockage of blood flow to the heart muscle. In some cases, there is severe blockage of the arteries, which limits the blood flow during times of physical stress – such as running, brisk walks, swimming etc. In this case, there is no plaque rupture, and is called angina pectoris – for chest pain.
The heart is a muscular pump and relies on a constant supply of blood – which carries essential nutrients and oxygen to continue to function. From the moment we are are born, plaque – also know as hardening of the arteries begins to accumulate. This process continues throughout our life and by the time we get to 60 years old, we may have
varying degrees of plaque build up inside our arteries.
This process may happen at a faster rate if we add additional stressors such as
hypertension, diabetes, high cholesterol, cigarette smoking. In some cases, you may have a genetic predisposition to having more aggressive plaque build up at a younger age. In most cases, this plaque build up is silent – that is, it doesn’t create any symptoms or signs, and testing may not show anything abnormal. Minor plaque build up which does not cause more than 70% blockage of the coronary artery typically does not produce any symptoms or signs.
Coronary artery disease will produce symptoms when the blockage in the artery is 70% or more, or if the plaque ruptures ( breaks) leading to clot formation, and sudden
blockage of blood flow close to 100%.
So there are three scenarios that may occur as a consequence of blocked arteries
1. No symptoms – Minor blockage, less than 70% blockage and no plaque rupture
2. Chest pain on exertion – example brisk walks or climbing stairs or during sports. Typically while resting, or doing minimal exertion, there is no chest pain, but may experience chest pain while walking fast, or climbing stairs. This is considered Stable Angina Pectoris. Major blockage with at least 70% obstruction of blood flow – typically produces chest pain when you exert yourself.
3. Chest pain at rest – while lying or sitting, or doing very light activity such as bathing or other activities of daily living. Minor or major blockage WITH plaque rupture – this usually causes chest pain at rest – while sitting or lying down, or doing minor exertion, that would not have produced pain in the past. This may be either Unstable Angina Pectoris or a Myocardial infarction (heart attack). This scenario is a medical emergency and requires a visit to the nearest emergency room.
To summarize – blocked arteries may cause NO symptoms, chest pain with activity or chest pain while doing nothing.
Chest pain
This is the most common symptom that a person suffering a heart attack will experience. The pain is usually described as heaviness or pressure in the centre or to the left of the
chest and may extend to the neck, jawline, or left shoulder or even down the left arm. It may sometimes give numb feeling down the left arm. The pain usually lasts for more
than 10 minutes and you may experience shortness of breath and or palpitations along
with the chest pain. Sometimes the pain may be felt as a burning sensation and less
frequently as sharp or sticking sensation, or tightness. Sometimes the pain or discomfort is mistaken for indigestion.
Do NOT make that mistake. Any chest pain in a person 40 years or older, especially with history of diabetes, hypertension , cigarette smoking, high cholesterol, family history of early coronary artery disease – is cause for concern.
If the chest pain lasts more than 10 minutes, and fits the description above, it is a
MEDICAL EMERGENCY. Do not self-treat with antacid and “watch it”. This is a sign you should call for help – best case scenario call an ambulance or get someone to drive you to the emergency room.
A note about heart attacks in women, diabetics and the elderly.
Women, diabetics and the elderly are notorious for having heart attacks with no
symptoms or atypical symptoms. They may sometimes do not experience the heavy
chest pain in the centre of the chest, but may only experience vague numbness in the arm, or neck, sometimes just shortness of breath or a feeling of dread. In some instances, may feel light headed or may faint.
In any of these circumstances with unexplained symptoms – it is reasonable to have your doctor check for a heart attack with an ECG and some blood work after careful review of your history and detailed examination.
Next we will discuss how we confirm the presence of blocked arteries and make the
diagnosis of a myocardial infarction or angina
A common question I get is “How do I know I have a heart problem”? Today, we will explore the common symptoms that may indicate that you have a heart problem.
Before we get into the specific symptoms that you may experience, one key point to remember, is that heart disease may be silent, and so regular check-up with your family physician is a good way to determine this. This is especially true for younger persons. At this time of year, as school children go on holidays, and parents grapple with all of the expenses of the summer break and back-to school preparations, the “Back-to-school Medical” is one big item on the agenda.
The “Back-to-School Medical” is probably the most important thing that you can do for your child, and it should not be short-changed. Do not ask a “doctor friend” to just sign the child’s form without actually examining the child. This exercise, that parents find annoying, expensive can make the difference between finding out your child has a health condition, or collapsing on the field at school from un-detected heart or other health condition. We will spend some time on the “Back-to-School Medical” in the future, but for today, suffice it to say, don’t scrimp. Save on that expensive book bag and get the child examined properly!
For older persons, who do not have any symptoms it is recommended that you get a medical examination at age 20 years with your family doctor and every five (5) years thereafter if this baseline medical is normal. This medical examination should include the following:
For persons who have heart disease, the symptoms that one might experience include
Shortness of Breath
Shortness of breath is often described as breathing faster than usual, or having difficulty catching one’s breath. There are certain circumstances under which shortness of breath will be “normal”, for example during or after physical exertion such as climbing flight of stairs, running, brisk walking, swimming, or playing a strenuous sport. Shortness of breath becomes significant if it occurs while sitting, or lying down, or if there is a change in your level of fitness. For example if you were able to climb a flight of stairs without feeling short of breath and now you have to stop several times to catch your breath before you get to the top.
While shortness of breath may indicate the presence of significant heart disease, it may also indicate the following
It is therefore very important that you see your family physician to explore some of these possibilities, before assuming it is a heart problem
Chest pain
Chest pain may be caused by several different conditions
Chest pain that is likely to be coming from the heart may be due to Coronary Artery disease(poor circulation to the heart) known as Angina or Inflammation of the lining of the heart – called pericarditis. Angina pain tends to have the following characteristics
Usually just below the breast plate
Heavy, or pressing feeling
Usually brought by exertion but may occur at rest
If you have been experiencing this type of pain, you need to visit your physician.
If you experience chest pain at rest, which fits these criteria, this is considered a medical emergency and should be treated as such! You should call for help and get someone to drive you to the ER or call an ambulance. It could mean that you are having a heart attack. Chest pain emergency if
A heart attack, or suspected heart attack is a medical emergency. You will need to have an urgent ECG and blood tests to confirm, or rule out the heart attack, or other potentially life-threatening causes of persistent chest pain such as clot on the lung or pulmonary embolism or tear in the major artery (Aortic dissection).
Part II – Palpitations, Fainting and Cough
Palpitations
A palpitation is the sensation that the heart is beating faster or stronger or an increased awareness of your heart beat, or that the heart is “skipping a beat”. Under normal circumstances, the heart beats in the background and we are not usually aware that it is there. It is “normal” to feel the heart beat stronger during or after physical exertion, as it is working harder to pump blood around the body to meet the increased demands that exercise places for oxygen and other nutrients.
If you notice palpitations as described, while you are sitting, or lying down, or if you get these symptoms long after exercise has stopped, or you feel dizzy or light-headed during this time, it may indicate a heart problem. Palpitations may be an indication that your heart rhythm may not be normal – what we call an arrhythmia – abnormal or irregular beating of the heart. Occasional skipping of the heart beat at rest, without the accompanying symptoms of chest pain or light-headedness may be an indication of and extra-heart beat. Usually after this extra heart beat, the timer in the heart “re-sets” itself so you may feel a little pause right after, like there is no heart beat, and then a strong beat. This can be “ normal” for up to 30% of normal persons. It is important though to have it checked out with your physician.
Otherwise from heart disease, palpitations may be an indicator of another general medical problem such as Anemia (low blood count) or an overactive Thyroid gland.
There are also some foods, drinks and over-the-counter medications that have stimulants, and may trigger palpitations. It is recommended that you cut these from your diet or treatment plan if palpitations are bothersome to you.
See your doctor for palpitations if
Your doctor will take a detailed history and examination, and an ECG should be done, with expert interpretation. Depending on these findings, the doctor may refer you to a cardiologist for further testing which may include additional tests such as an Echocardiogram (Ultrasound of the heart) or 24 Hour Holter ( 24 hour ECG recording).
Fainting (Syncope) or Near-fainting (Pre-syncope) and Dizziness
Fainting is a sudden, brief loss of consciousness, usually lasting a few seconds. It usually results with the person falling to the floor with prompt recovery of consciousness when the person is lying or sitting down. Loss of consciousness that is longer than a few seconds is not truly a fainting spell and could be seizure or other indication of a brain problem. Some persons may not experience loss of consciousness, but may feel light-headed, like they are going to black out, but do not actually black out. This is referred to as near-fainting.
This is to be distinguished from dizziness which in medical language we call vertigo and is classically described as a feeling of being unsteady, or that the person is spinning relative to the room, or the room is spinning. Dizziness (vertigo) is more an indication that the balance mechanism is out of whack and could indicate an inner/middle ear problem or brain problem affecting the balance mechanism.
Fainting or near fainting may be what is referred to a simple faint (vaso-vagal syncope) – which has no underlying heart problem, can be due to dehydration or other easily remediable fixes. A simple faint, does not usually indicate a heart problem, but if the person who has fainted has never had a medical examination, it should be done and then the person can be re-assured if normal. When not due to vaso-vagal syncope (or simple faint), fainting may indicate the following potentially serious underlying heart conditions
Any episode of fainting should be reviewed by a physician
Cough
A cough that is lasting more than a few days, and not in association with flu-like symptoms may be an indication of heart disease, particularly heart failure. A cough occurs in heart failure, when the heart is not pumping strong enough, it leads to a build-up of fluid in the lungs. The cough associated with heart failure has the following features
As a reminder – if you experience any of these symptoms and are concerned – see your family physician right away. For chest pain lasting more than 10 minutes, for persons over 40 years old, especially with any underlying medical problems such as high cholesterol, diabetes or hypertension – and Emergency Room visit is a must. Do not wait to see your physician during regular hours, or “watch it”.